Screening and Assessment Guidelines
Preconception
Why is screening important?
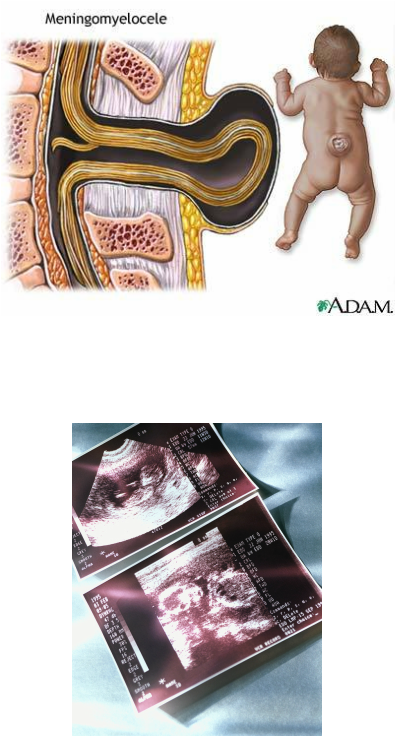
Folic acid supplementation (at least 400 µg for childbearing age and up to 600 µg for pregnant females) to prevent neural tube birth defects such as spina bifida.
Women should receive proper immunizations to promote health and prevent disease. Please note these are for PRECONCEPTION not pregnancy. Check with a physician first.
Screening for certain diseases is paramount for a healthy pregnancy.
- Seeking medical care prior to conception may improve pregnancy outcomes as well as health of the woman.
- Women planning to become pregnant (and even those who are not) should visit a physician at least once a year to ensure adequate health for themselves and the fetus.
Folic acid supplementation (at least 400 µg for childbearing age and up to 600 µg for pregnant females) to prevent neural tube birth defects such as spina bifida.
Women should receive proper immunizations to promote health and prevent disease. Please note these are for PRECONCEPTION not pregnancy. Check with a physician first.
- Rubella to prevent congenital defects.
- Hepatitis B for at-risk women to prevent liver disease.
- Inactivated influenza
Screening for certain diseases is paramount for a healthy pregnancy.
- HIV/AIDS (may be passed to fetus if anti-retroviral therapies not followed)
- Diabetes (may promote macrosomia or glucose intolerance in fetus)
- Sexually transmitted diseases (may promote ectopic pregnancy, fetal anomalies)
- Depression (may increase chances of postpartum depression)
- Hypothyroidism (prevent neurological defects, cretinism with correct iodine supplementation)
- Smoking cessation (reduces negative perinatal outcomes)
- Alcohol intake cessation (reduces fetal alcohol disorders and other effects: mental retardation, hyperactivity, seizures)
- Recreational drug use cessation
Pregnancy
Visit Schedule
- Initial visit before 10 weeks
- 14-16 weeks
- 24-28 weeks
- 32 weeks
- 36 weeks
- 38 weeks
- 40 weeks
- Weekly until delivery, up to 42 weeks
- High risk patient will require closer follow up
First Trimester
Initial visit
- Pregnancy test to confirm pregnancy
- Health history
- OB history
- Menstrual history / LMP
- Sexual history including sexually transmitted diseases / risk for HIV
- Contraceptives
- Medical and surgical history
- Recent or current infections
- Genetic history / family history
- Immunization status
- Current medications / allergies
- Teratogenic exposures
- Socio-demographic data
- Pregnancy readiness including knowledge and feelings toward pregnancy
- Nutrition status and weight
- Housing and financial issues / concerns
- Tobacco, alcohol and drug use history
- Signs of abuse including physical, emotional and sexual
- Complete physical, including lactation assessment
- Calculate due date
- Assess for complications such as morning sickness
First Trimester Screening and Tests
Second Trimester
Physical Assessment
- Weight
- Blood pressure
- Auscultation of fetal heart tones
- Measurement of fundal height
- Assess for complications such as vomiting, heart burn or others
- Signs of depression
- Provide support
- Signs of abuse or neglect
- Continue to address readiness for childbirth, breastfeeding and expectations
- Referral to appropriate community resources to assist in meeting educational needs (prepared childbirth classes, breastfeeding classes, classes for first time parents on caring for infants, car seat safety, etc)
- Follow up on modifiable risks that patient is addressing
Second Trimester Testing and Screening
Third Trimester
Physical Assessment
Weeks 32-36 visit
Weeks 32-36 visit
- Weight
- Blood pressure
- Auscultation of fetal heart tones
- Measurement of fundal height
- Same as above
- Include measurements of cervical effacement and dilation
- Group B strep swabs performed again
- Signs of depression
- Provide support
- Signs of abuse or neglect
- Continue to address readiness for childbirth, breastfeeding and expectations
- Give opportunity to ask questions